Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding leads ecg placement is essential for accurate cardiac diagnostics. A small error can lead to misdiagnosis—here’s how to get it right every time.
Leads ECG Placement: The Foundation of Accurate Heart Monitoring

Electrocardiography (ECG or EKG) is one of the most widely used diagnostic tools in cardiology. It measures the electrical activity of the heart and helps detect arrhythmias, ischemia, infarction, and other cardiac conditions. At the heart of this diagnostic precision lies proper leads ecg placement. Incorrect lead positioning can distort waveforms, mimic pathology, or mask real issues—leading to clinical errors.
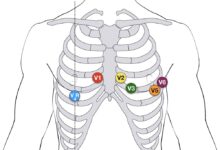
The standard 12-lead ECG uses ten electrodes placed on the limbs and chest to generate twelve different electrical views of the heart. These leads are divided into limb leads (I, II, III, aVR, aVL, aVF), augmented limb leads, and precordial (chest) leads (V1–V6). Each lead provides a unique angle of the heart’s electrical vector, making correct placement non-negotiable for diagnostic integrity.
“A mispositioned ECG lead can look like a myocardial infarction on paper,” says Dr. Richard Wesley, a cardiologist at Johns Hopkins Medicine. “That’s how critical proper leads ecg placement really is.”
Why Proper Leads ECG Placement Matters Clinically
Accurate leads ecg placement ensures that the recorded electrical signals reflect true cardiac activity. Misplaced electrodes can cause:
- False ST-segment elevation or depression
- Misinterpretation of axis deviation
- Inaccurate R-wave progression in precordial leads
- Masking of bundle branch blocks or ventricular hypertrophy
For example, placing V1 and V2 too high can mimic right bundle branch block patterns, while misplaced V4–V6 can simulate lateral myocardial infarction. These errors not only delay correct diagnosis but may lead to unnecessary interventions such as angiography or anticoagulation therapy.
Standard Guidelines for Leads ECG Placement
The American Heart Association (AHA) and the Association for Advancement of Medical Instrumentation (AAMI) have established standardized protocols for leads ecg placement. These guidelines ensure consistency across healthcare settings and reduce inter-operator variability.
Limb leads are placed on the right and left wrists and ankles (or upper arms and lower legs if limb movement interferes). The chest (precordial) leads follow a specific anatomical roadmap:
- V1: 4th intercostal space, right sternal border
- V2: 4th intercostal space, left sternal border
- V3: Midway between V2 and V4
- V4: 5th intercostal space, midclavicular line
- V5: Same horizontal level as V4, anterior axillary line
- V6: Same level as V4 and V5, midaxillary line
Adherence to these landmarks is crucial. Even a shift of 1–2 intercostal spaces can alter ECG morphology significantly.
Common Errors in Leads ECG Placement and Their Consequences
Despite clear guidelines, errors in leads ecg placement are surprisingly common. Studies show that up to 40% of ECGs have at least one lead misplaced. These mistakes often go unnoticed but can profoundly affect patient outcomes.
One of the most frequent errors is incorrect identification of the 4th intercostal space. Clinicians sometimes count ribs from the top down incorrectly, placing V1 and V2 too high or too low. This leads to abnormal R-wave progression and can mimic anterior myocardial infarction.
Misplaced Precordial Leads: A Diagnostic Trap
Among all leads ecg placement errors, misplaced precordial leads are the most clinically significant. V1 and V2 are particularly vulnerable due to their proximity to the right ventricle and atria.
When V1 is placed too high (e.g., 3rd intercostal space), it may record atrial activity more prominently, leading to exaggerated P-waves that resemble atrial enlargement. Conversely, placing V1 too low can bury the R-wave, mimicking poor R-wave progression seen in anterior infarction.
V4 placement is another common pitfall. It should be located at the 5th intercostal space along the midclavicular line. However, in obese patients or those with large breasts, this point can be difficult to locate. Misplacement laterally or superiorly alters the transition zone and distorts QRS morphology.
According to a 2020 study published in Journal of Electrocardiology, incorrect V4 placement was found in 32% of ECGs reviewed, with 18% showing clinically significant changes in ST segments.
Limb Lead Reversals: Silent but Dangerous
Limb lead reversals are another category of leads ecg placement error. The most common is right-left arm reversal, which can mimic dextrocardia or lead to incorrect axis calculation.
Signs of right arm-left arm reversal include:
- Lead I showing negative P waves, QRS complexes, and T waves
- Lead aVR becoming upright instead of inverted
- Leads II and III switching places
These changes can be mistaken for complex congenital heart disease or incorrect lead wiring. While experienced interpreters may recognize the pattern, in urgent settings, this can delay care.
Other reversals—like left arm-left leg (LA-LL)—can mimic inferior wall myocardial infarction due to inverted QRS in leads II, III, and aVF. Always verify electrode placement before concluding pathology.
Step-by-Step Guide to Correct Leads ECG Placement
Performing a 12-lead ECG with accurate leads ecg placement requires both knowledge and technique. Follow this step-by-step protocol to ensure precision.
Begin by positioning the patient supine, relaxed, with arms at their sides. Expose the chest fully and identify anatomical landmarks under good lighting. Use palpation—not estimation—to locate intercostal spaces.
Locating Key Anatomical Landmarks
The accuracy of leads ecg placement hinges on correctly identifying anatomical landmarks. Start with the angle of Louis (sternal angle), which sits at the junction of the manubrium and body of the sternum. This landmark corresponds to the 2nd rib and serves as your reference point.
From the angle of Louis, slide your fingers laterally to feel the 2nd rib, then count down to the 4th intercostal space. This is where V1 and V2 go—right and left sternal borders, respectively.
For V4, find the 5th intercostal space at the midclavicular line. This is the imaginary line extending down from the midpoint of the clavicle. In women with large breasts, lift the breast tissue gently to place the electrode directly on the chest wall, not on the breast itself.
Placing Chest and Limb Electrodes Accurately
Once the precordial landmarks are identified, place the electrodes in order: V1, V2, V4, V3, V5, V6. This sequence prevents confusion and ensures symmetry.
- V1: 4th ICS, right sternal border
- V2: 4th ICS, left sternal border
- V4: 5th ICS, midclavicular line
- V3: Midway between V2 and V4
- V5: Same horizontal level as V4, anterior axillary line
- V6: Same level, midaxillary line
Limb electrodes should be placed on the fleshy parts of the limbs—distal forearm and lower leg—to minimize motion artifact. Avoid bony prominences and areas with muscle tremor.
Ensure all skin is clean, dry, and free of oils or lotions. Shave excessive hair if necessary. Poor skin contact increases impedance and degrades signal quality.
Special Considerations in Leads ECG Placement
While standard leads ecg placement works for most patients, special populations require modifications. These include pediatric patients, obese individuals, pregnant women, and those with anatomical abnormalities.
Adapting the technique ensures diagnostic accuracy without compromising patient comfort or safety.
Leads ECG Placement in Pediatric Patients
Children have smaller thoraces and different heart positions relative to adults. Although the same 12-lead system is used, electrode placement must be scaled accordingly.
In infants and young children:
- Use smaller electrodes designed for pediatric use
- Place precordial leads closer together, maintaining anatomical proportion
- V1 and V2 remain at the 4th ICS, but V4–V6 may be shifted slightly depending on chest size
Always label the ECG as “pediatric” to alert interpreters of potential normal variants like upright T waves in V1 or right axis deviation.
Adjustments for Obese and Pregnant Patients
Obesity can obscure anatomical landmarks, making leads ecg placement challenging. Subcutaneous fat displaces the heart and alters ECG waveforms. In these cases:
- Use ultrasound guidance if available to confirm heart position
- Ensure electrodes are placed on the chest wall, not on adipose tissue folds
- Consider using adhesive electrodes with stronger gel for better contact
In pregnant women, the diaphragm is elevated, shifting the heart upward and to the left. This can cause left axis deviation and poor R-wave progression. To compensate:
- Place V1 and V2 at the 3rd ICS if the 4th is inaccessible
- Adjust V4–V6 slightly higher if needed
- Document pregnancy status on the ECG report
These adjustments help maintain diagnostic reliability despite physiological changes.
Impact of Leads ECG Placement on Diagnostic Accuracy
The clinical impact of incorrect leads ecg placement cannot be overstated. A study from the University of California, San Francisco, found that 27% of ECGs with misplaced leads led to altered clinical decisions, including unnecessary hospital admissions or missed acute coronary syndromes.
One notable case involved a 58-year-old male whose ECG showed ST elevation in leads V1–V3. Suspected anterior STEMI, he was rushed to the cath lab—only to discover that V1 and V2 were placed in the 2nd intercostal space. After repositioning, the ST elevation resolved, revealing a normal ECG.
How Misplacement Mimics Myocardial Infarction
Incorrect leads ecg placement can simulate the classic signs of myocardial infarction:
- Poor R-wave progression due to high V1/V2 placement
- ST elevation in right precordial leads mimicking anterior MI
- Inverted T waves in V1–V3 resembling ischemia
These patterns are often labeled as “pseudo-infarct” patterns. They arise not from pathology but from altered vector projection caused by electrode misplacement.
For instance, placing V4 too laterally shifts the transition zone posteriorly, reducing R-wave amplitude in V3 and V4—exactly what’s seen in anterior infarction.
Effect on Cardiac Axis and Rhythm Interpretation
The electrical axis of the heart is determined by the net direction of depolarization, calculated using limb leads. Errors in leads ecg placement, especially limb reversals, can shift the apparent axis by 30–60 degrees.
Right arm-left arm reversal causes extreme left axis deviation on paper, while left arm-left leg reversal mimics inferior infarction with upright QRS in aVR. These artifacts confuse rhythm interpretation and may lead to incorrect classification of arrhythmias.
Always double-check lead placement when axis deviation or unusual limb lead patterns appear suddenly without clinical correlation.
Best Practices for Ensuring Accurate Leads ECG Placement
Ensuring correct leads ecg placement requires more than just following a checklist—it demands attention to detail, proper training, and a culture of quality assurance.
Healthcare institutions should implement standardized ECG protocols, regular staff training, and periodic audits of ECG quality.
Training and Certification for ECG Technicians
ECG technicians are the frontline guardians of leads ecg placement accuracy. Comprehensive training programs should include:
- Anatomy and physiology of the heart’s electrical system
- Step-by-step electrode placement techniques
- Recognition of common errors and their ECG manifestations
- Hands-on practice with mannequins and live patients
Certification programs like those offered by the National Healthcareer Association (NHA) or the Cardiovascular Credentialing International (CCI) validate competency and promote best practices.
Regular refresher courses help maintain skill levels, especially in high-turnover environments like emergency departments.
Quality Control and ECG Audits
Hospitals and clinics should conduct routine ECG audits to assess leads ecg placement accuracy. A random sample of ECGs can be reviewed by cardiologists or ECG specialists for:
- Correct anatomical placement
- Presence of artifact or noise
- Consistency with patient history
- Signs of lead reversal or misplacement
Feedback should be provided to technicians, and corrective actions taken when error rates exceed acceptable thresholds (e.g., >10%).
Some institutions use digital ECG systems with built-in placement verification algorithms. These tools flag potential errors before the ECG is finalized, reducing preventable mistakes.
Technological Advances in Leads ECG Placement
Technology is playing an increasing role in improving the accuracy of leads ecg placement. From smart electrodes to augmented reality, innovations are helping clinicians get it right the first time.
These tools are especially valuable in fast-paced environments where time pressure increases the risk of error.
Smart Electrodes and Real-Time Feedback Devices
Newer ECG systems incorporate smart electrodes that detect poor contact or incorrect positioning. Some devices provide real-time audio or visual alerts if impedance is too high or if lead reversal is detected.
For example, the Philips PageWriter TC70 includes a lead placement advisor that checks for reversals and notifies the operator before recording.
These systems reduce human error and improve first-time pass rates, especially among less experienced staff.
Augmented Reality and Mobile Apps
Augmented reality (AR) apps are emerging as training tools for leads ecg placement. Using a smartphone or tablet camera, AR overlays anatomical landmarks and electrode positions onto the patient’s body in real time.
Apps like “ECG Lead Placement AR” guide users through each step, ensuring V1 is at the 4th ICS and V4 at the midclavicular line. These tools are particularly useful for students and new technicians.
While not yet standard in clinical practice, they represent a promising direction for reducing placement errors.
Legal and Ethical Implications of Incorrect Leads ECG Placement
Mistakes in leads ecg placement aren’t just clinical—they can have legal consequences. Misdiagnosis due to technical error may constitute negligence, especially if proper protocols were not followed.
In malpractice cases, defense attorneys often scrutinize ECG technician training, equipment maintenance, and institutional policies.
Medical Malpractice Risks
If a patient suffers harm due to a misdiagnosed MI or arrhythmia caused by incorrect leads ecg placement, the healthcare provider may be held liable. Courts expect adherence to established standards of care, including proper electrode positioning.
Documentation is key. Always note any difficulties with placement (e.g., “V4 placed at 5th ICS, midclavicular line, after lifting breast tissue”) to demonstrate due diligence.
Ethical Responsibility in Patient Care
Accurate leads ecg placement is an ethical obligation. Patients trust clinicians to perform tests correctly. Cutting corners or rushing through an ECG violates that trust and compromises care quality.
Healthcare professionals must prioritize precision over speed, especially in critical settings like chest pain evaluation.
As the Hippocratic Oath reminds us: “First, do no harm.” Proper technique is a fundamental part of that promise.
What is the correct placement for V1 in leads ecg placement?
V1 should be placed in the 4th intercostal space at the right sternal border. This position ensures accurate recording of right ventricular and atrial activity. Misplacement can lead to false diagnoses such as right bundle branch block or anterior myocardial infarction.
How does limb lead reversal affect ECG interpretation?
Limb lead reversal, especially right-left arm swap, inverts waveforms in lead I and can mimic dextrocardia or incorrect axis deviation. It may also cause leads II and III to switch, leading to misinterpretation of inferior wall activity. Always check for negative P waves in lead I as a clue.
Can incorrect leads ecg placement cause a false diagnosis of heart attack?
Yes, absolutely. Misplaced precordial leads—especially V1–V3—can create poor R-wave progression or ST-segment changes that mimic anterior myocardial infarction. This can lead to unnecessary interventions like thrombolysis or catheterization.
What should I do if anatomical landmarks are hard to find?
If landmarks are obscured (e.g., due to obesity or trauma), use palpation carefully, consider ultrasound guidance, or document the challenge clearly. Never guess—imprecise placement compromises diagnostic value.
Are there differences in leads ecg placement for men and women?
The anatomical placement is the same, but in women with large breasts, V3–V6 should be placed on the chest wall beneath the breast tissue, not on the breast itself. This prevents signal attenuation and distortion.
Proper leads ecg placement is the cornerstone of reliable ECG interpretation. From identifying anatomical landmarks to avoiding common errors, every step impacts diagnostic accuracy. Whether you’re a student, technician, or physician, mastering this skill prevents misdiagnosis, improves patient outcomes, and upholds professional standards. With training, technology, and vigilance, we can ensure every ECG tells the true story of the heart.
Further Reading: